Flashes & Floaters
Overview
Floaters have many appearances. They are usually most prominent when looking against a bright background.
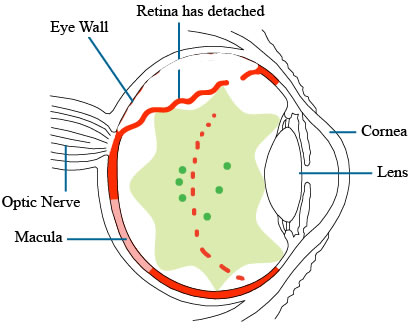
Flashes and floaters are very common. Having them does not always mean a torn retina. On the other hand, it is definitely a good idea to see a retina specialist if you are developing any new flashes and floaters. A torn retina can usually be treated by a laser. If you notice a shadow or a shade or a thumbprint in your vision, this can mean your retina has detached, and you may need surgery to repair the retina.
Flashes in Detail
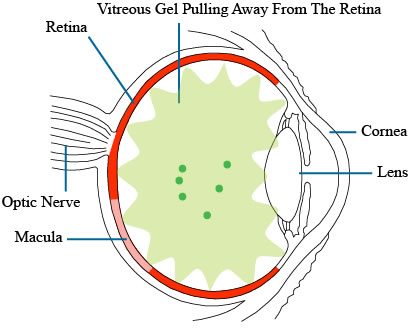
Flashes in retinal detachment are usually split-second or few-seconds at a time. They can be like streaks of lightning, noticeable especially in a dark room. They can occur randomly at different times of the day. They can be quite alarming. They usually occur at the side of the vision. Sometimes you can induce a flash or a streak of light by moving your eyes from side to side quickly.
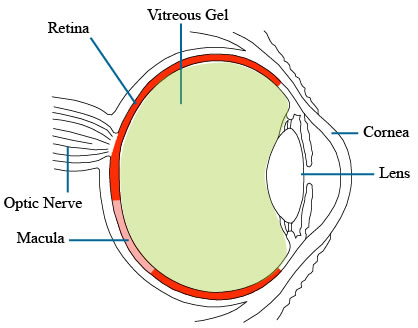
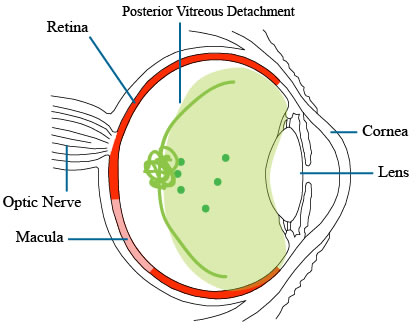
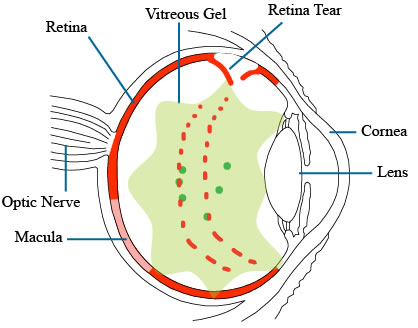
Flashes like this may mean the vitreous gel inside the eye is shrinking and coalescing and pull away from the retinal surface. If the gel can successfully pull away from the retina, then the condition becomes harmless, and is called a posterior vitreous detachment. It is only when the gel does not pull cleanly away from the retina that a retinal detachment may develop.
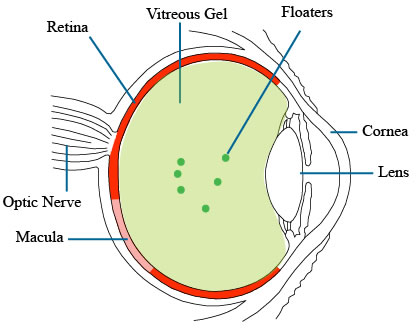
Floaters in Detail
If you look at a bright background such as the blue sky or a computer screen, you can often notice some normal floaters. They are usually a few in number. Floaters can look like a web, a string or a circle, or a bunch of dots. Floaters usually move around somewhat randomly when you eye moves. Normal floaters usually don’t change much. Over the years, you may accumulate more floaters.
By contrast, floaters in retinal detachment are often sudden and new. They can look like one piece of large web or strand, or there can be thousands of tiny little floaters. Yours can look like something else. The tiny little floaters are actually red blood cells or pigment cells, and they suggests a higher chance that there is a retinal tear or detachment. However, it is important to not completely rely on the absence of floaters. Sometimes the floaters in retinal detachment can be subtle. Occasionally a retinal detachment can develop without any floaters.
Posterior Vitreous Detachment
Posterior Vitreous Detachment (PVD) is usually an age-related event. It is very common after age 60, but it can occur at a younger age, especially if you are near-sighted. A PVD can happen after a minor ocular injury or recent eye surgery like a cataract operation. It usually means the vitreous gel has matured, and shrunken and pulled away from the retina. A new PVD is often associated with new floaters or flashes. If the gel shrinkage or pulling away is clean from the retina, then the prognosis is usually good. However, the vitreous gel can be adherent to the retina, and then it can cause problems such as vitreous hemorrhage, retinal detachment, epiretinal membrane, or macular hole. So if you notice new floaters or flashes of light or distorted central vision, you should see your eye doctor or a retina specialist.
What Happens After You See Your Doctor
If you are diagnosed with a PVD without any retinal tear or detachment. That is good news. However, in the first few weeks, it is possible that the vitreous gel may pull more and still end up tearing or detaching the retina. So if you have more floaters, especially if there are suddenly many tiny ones, you should have your retina checked again. You may also want to get your retina checked again if you have more flashes, but flashes can go on for a few weeks before it starts subsiding. If you notice a shadow or a shade or a thumbprint in your vision, this may mean your retina has detached and you may need surgery to repair that. Also, since PVD is usually an age-related event, the other eye may develop the same thing within a year or so.
A PVD can seem very bothersome at first. However, after a few months, most patients will adapt successfully to their floaters. It usually seems to “go away” in a few months, even though it is still visible to the doctor when looking into the eye. However, some patients can find the floaters extremely distracting and debilitating. The floaters may interfere with many activities of daily living, such as reading or driving or working. In those situations, a surgical procedure called Pars Plana Vitrectomy may be the best option to to remove the vitreous floaters. In some cases, a YAG laser vitreolysis procedure may be performed. All of these procedures have some risks, and may not get rid of the floaters 100%. It is best to try to adapt and adjust to the floaters first, if at all possible.